Explore how Metformin works beyond diabetes. Buy Metformin online safely and discover its roles in weight loss, energy, and aging.
| Dosage Options | Price for 60 pills | Where to Buy Online |
|---|---|---|
| Metformin 500mg, 850mg | $44.89 | Online Pharmacies |
Content:
- Metformin — More Than Just a Diabetes Drug: A Modern Perspective
- How Metformin Works: Its Impact on Glucose, Insulin, and Mitochondria
- Where to Buy Metformin Online: Prices, Pharmacies, and How to Avoid Fakes
- How to Start Taking Metformin Properly: Dosage, Schedule, and Adaptation
- Metformin for Weight Loss: Scientific Evidence and Real-World Cases
- Metformin Side Effects: Common Issues and How to Minimize Them
- Is Metformin Compatible with Other Medications? Interactions and Risks
- Metformin Against Insulin Resistance: Mechanism, Indications, and Effectiveness
- Can You Take Metformin Without Diabetes? An Endocrinologist’s Answer
- Metformin and Physical Exercise: Can It Support Your Workouts?
- The Anti-Aging Effect of Metformin: Myth or Biomedical Breakthrough?
Metformin — More Than Just a Diabetes Drug: A Modern Perspective
Metformin first gained popularity as a reliable first-line therapy for type 2 diabetes because it lowers blood glucose without stimulating the pancreas to generate more insulin. The safety profile — few lows, little side effects, and decades of strong data — made it a popular prescription all across the world. However, focusing just on its glycemic impact is like to savoring a single note in a symphony.
Over the last fifteen years, researchers discovered that metformin quietly modifies numerous metabolic "knobs" at the same time: it lowers liver glucose production, promotes muscles to absorb sugar more efficiently, and even reduces low-grade inflammation associated with insulin resistance. These discoveries opened the door for researchers to look into metformin's potential use outside of diabetes.
Physicians are also experimenting with low-dose regimens for prediabetes, polycystic ovarian syndrome (PCOS), and persistent weight gain induced by insulin resistance. Early research suggests that metformin may act as a metabolic "reset"— nothing magical, simply a steady hand regulating blood sugar surges into smoother waves, so suppressing appetite and fat formation.
- Blunts liver glucose production, reducing fasting blood sugar
- Improves insulin sensitivity in muscle and fat tissue
- Lowers circulating insulin levels, curbing hunger peaks
- Dampens chronic inflammation markers (e.g., CRP)
- Activates AMPK, a cellular “energy sensor” tied to longevity research
The AMPK link spurred scientists to investigate if the medicine may postpone age-related illnesses. TAME (Targeting Aging with Metformin) is a big project designed to test that notion by determining whether long-term users have fewer cardiovascular events, cancers, or cognitive decline. Until the evidence is in, metformin is an intriguing competitor, but not a proven elixir of youth.
Finally, affordability is crucial. Metformin, which costs approximately a dollar per day — or less for generics — stands out in a market where cutting-edge metabolic drugs can cost hundreds of dollars per month. This cost-effectiveness trade-off keeps doctors interested in scalable, population-level approaches to combating obesity and metabolic syndrome.
How Metformin Works: Its Impact on Glucose, Insulin, and Mitochondria
Metformin's trip begins in the stomach. After swallowing a pill, a portion of the dosage remains in the intestinal wall, delaying glucose absorption and resulting in flatter, shorter post-meal sugar peaks.
The next destination is the liver. Metformin inhibits an enzyme chain that usually directs the liver to release stored glucose into the circulation. When that tap is turned down, fasting sugar levels drop naturally rather than being driven down by more insulin.
Third, the medication communicates with muscle cells, urging them to draw more glucose from the blood for fuel. Consider turning on dormant "fuel pumps" so muscles may munch on sugar rather than having it float about unused.
AMPK, often known as the cell's energy monitor, is the driving force behind these actions. Metformin stimulates AMPK into a "on" state, causing cells to consume available energy and produce less new fat. The end consequence is a little increase in calorie consumption, which is scarcely detectable on a daily basis but significant over time.
Metformin marginally delays the electron transport chain inside mitochondria, the cell's power factories. That modest brake informs the cell, "Energy is scarce; be efficient," which aligns with AMPK's overall push for enhanced metabolism and lower oxidative stress.
Because insulin levels decline alongside glucose, cravings caused by fast sugar fluctuations subside. For many patients, this means eating lesser quantities without relying on willpower, which helps with weight loss attempts.
Finally, metformin's minimal risk of hypoglycemia (dangerously low blood sugar) makes it suitable for beginners. It complements rather than disrupts the body's natural rhythms, which is why doctors frequently use it as the first chapter in a patient's metabolic reset plan.
Where to Buy Metformin Online: Prices, Pharmacies, and How to Avoid Fakes
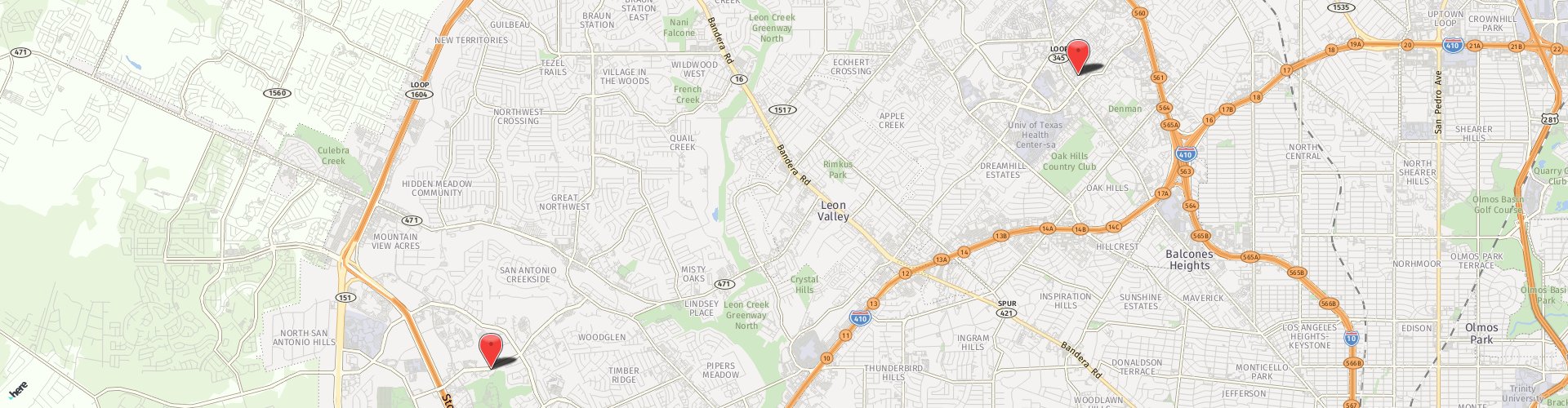
Purchasing Metformin online can save you time and, in many situations, a significant amount of money—especially if you live a long distance from a physical pharmacy if your insurance copay is high. In the United States, generic pills typically cost only a few dollars per month when a discount is applied, but the identical prescription at the corner shop may cost 10 times more. That price difference explains why "buy Metformin online" has become such a popular search term.
Prices vary even within recognized retailers. A 60-tablet supply of 500 mg extended-release Metformin costs roughly $18 at HealthWarehouse, whereas the same number of 850 mg tablets costs around $19. On Amazon Pharmacy, the cash price for 30 500 mg pills is $17, so if you double the amount, expect to pay around $34 for 60 tablets.
Below is a quick snapshot of typical online pricing.
| Pharmacy | 500 mg × 60 tabs | 850 mg × 60 tabs | Delivery Region |
|---|---|---|---|
| Stanley-Pills24 | $44.89 | $44.89 | Worldwide (tracked) |
| HealthWarehouse | ≈ $18 | ≈ $19 | USA only |
| Amazon Pharmacy | ≈ $34* | N/A | USA (Prime members) |
| Blink Health | $12–15 | $15–18 | USA (home delivery) |
| GoodRx Coupon** | as low as $2 | — | USA (local pickup) |
Shipping times are nearly as essential as the sticker price. E-pharmacies in the United States normally provide two to four days of delivery; international sellers frequently charge one to three weeks, with probable customs delays. Before making a payment, confirm the shipment method and tracking details.
When deciding which pharmacy is ideal for you, consider prescription requirements, accepted payment options, and whether you need immediate-release or extended-release medicines. Take special caution with returns: if a package arrives damaged or the imprint code seems "off," you should be able to return it without trouble.
Counterfeiting remains a major problem, especially on lightly controlled marketplaces. Stick to websites that show a valid pharmacy license or VIPPS seal, require a doctor's prescription, and offer pharmacist chat support. If any of these are missing, carry on.
A last sanity check: study the pill. Genuine Metformin tablets have thick score lines and a distinct imprint. Warning flags include powdery coating, illegible logos, and missing lot numbers. It's best to be safe than sorry, so photograph anything weird and report it.
How to Choose a Reliable Pharmacy for Buying Metformin Online
To attract customers, online shops typically provide free delivery, extra refills, or loyalty points. Nice extras, but begin with the basics: license, source openness, and data security.
Start by scrolling to the footer. Legitimate US websites include a NABP or VIPPS badge that leads to a verification page. In the EU, look for the green "common logo." The lack of license information is an immediate deal breaker.
Next, compare the prices. A minor discount compared to your local pharmacy is OK; a 95% markdown is not. Extreme discounts might suggest misplaced or fake products.
- No prescription required for a prescription drug
- Domain registered very recently (check WHOIS)
- No physical address or phone; only a web form
- Accepts crypto only, no credit-card chargebacks
- Promises “generic metformin without side-effects” (impossible)
- Poor grammar or pixelated logos on the site
Also, consider payment security. The checkout page should start with "https://" and have a padlock icon. If the padlock vanishes while you are entering card details, abandon the cart.
Finally, contact the drugstore over the phone or by email. Reputable providers react within one business day and can pinpoint the exact manufacturer from which they will ship. Silence — or copied-and-pasted responses — indicates that you should shop elsewhere.
Brand vs. Generic Metformin: Is It Worth Paying More?
When Metformin first made its way into pharmacies in the 1990s, Glucophage was the sole brand available. Patent expiration paved the way for generics, and costs plummeted overnight. Both formulations have the same active component (Metformin HCl) and must follow FDA bioequivalence guidelines, which mean the medicine enters your circulation at the same rate and concentration.
Why is the brand so expensive? Mostly marketing inertia and strict control over some extended-release technology. Patients who experienced GI discomfort with prior generics occasionally felt better on Glucophage XR, fueling the misconception that "brand works better." In actuality, most current generics employ the same polymer matrix.
| Feature | Brand (Glucophage & XR) | Generic (Metformin) |
|---|---|---|
| Active ingredient | Metformin HCl | Metformin HCl |
| FDA bioequivalent? | Yes (reference) | Yes (AB-rated) |
| Typical cost (500 mg × 60) | $250–300 (cash) | $10–20 with coupon |
| Formulations | Immediate & XR | Immediate, XR, sprinkle caps |
| Insurance coverage | Tier 3 (higher copay) | Tier 1 (lowest copay) |
For the vast majority of patients, generic Metformin offers the same benefits at a far cheaper cost. The only exception is if someone demands a specific extended-release delivery system and refuses to accept lower-cost alternatives—in which case, investing more may be justified.
Still unsure? Ask your doctor to write "dispense as written" for one month of brand XR and keep note of the negative effects. If there is no difference, switching back to generic might save you hundreds of dollars every year.
How to Start Taking Metformin Properly: Dosage, Schedule, and Adaptation
Starting Metformin is more about patience and strategy than brute force. The drug works best when you ease in gradually, let your gut adjust, and pair it with consistent mealtimes. Most prescribers begin with 500 mg once daily at the largest meal (usually dinner) to blunt the most pronounced overnight glucose rise. If stomach upset stays mild after one week, the dose steps up to 500 mg twice daily—breakfast and dinner.
For people whose fasting sugar is still climbing, a common next move is 850 mg in place of the 500 mg tablet at dinner. The larger tablet packs more punch but carries a slightly higher risk of GI rumble, so it’s usually introduced only after the body tolerates the lower dose.
- Week 1: 500 mg with your evening meal
- Week 2: 500 mg with breakfast and 500 mg with dinner
- Week 3–4: If targets unmet, switch dinner dose to 850 mg
- Maintenance: Adjust every 2‒4 weeks toward 1500–2000 mg per day, split into two or three meals, per clinician advice
The timing of food consumption is important. The most frequent adverse effect of Metformin is a queasy, gassy stomach. Taking each pill during a meal, rather than on an empty stomach, allows food to "cushion" the drug as it dissolves. Skipping breakfast and still taking the morning medication is a recipe for nausea.
Hydration also helps. Aim for a full glass of water with the dosage. Adequate fluid intake not only relieves GI discomfort, but it also counteracts the slight diuretic impact that some people experience during the first month.
The adaption phase typically lasts two to six weeks. Expect lighter bowel movements, a metallic taste, or a transient drop in appetite; these normally pass when gut flora and digestive enzymes rebalance. If cramps or diarrhea last more than two weeks, consult your doctor about reducing the titration or switching to extended-release pills.
Metformin does not require a fixed schedule; it can be taken with any significant meal, but consistency is key. Choose two anchor meals that you seldom skip (for example, 8:00 a.m. breakfast and 7:00 p.m. supper) and set phone reminders. Blood sugar levels become more predictable when dosages are administered at consistent times throughout the day.
Other medications might cause Metformin levels to rise or fall. Always keep your prescription list up to date so that your doctor can adjust dosages as required.
Finally, keep in mind that Metformin is a gradual and consistent glucose-lowering medication, not a quick fix. Most individuals notice the full benefit after 8-12 weeks of consistent dosage. Stick to the plan, note your fasting sugars weekly, and bring those figures to follow-up appointments for adjustments.
Which Form Is Better: Immediate-Release or Extended-Release Metformin?
Choosing between regular (immediate-release, IR) and extended-release (XR, ER) Metformin is a balancing act between cost, convenience, and stomach comfort.
Immediate-release shines when precise, meal-linked dosing is key—say, targeting a stubborn post-dinner glucose spike. Its two-to-three-times-daily schedule also allows flexible titration in 500 mg increments, useful if you’re sensitive to side-effects. The trade-off is a higher chance of GI upset, because each tablet dumps its payload within hours.
Extended-release tablets dissolve gradually over 24 hours, so most people take them once nightly (or twice if doses exceed 2000 mg). That slow drip cuts peak concentrations in the gut, slashing nausea and bathroom runs by roughly half in clinical studies. XR is a lifesaver for shift workers, breakfast-skippers, or anyone who hates mid-day pill alarms.
When does IR still win?
- Very tight budgets. Generic IR tablets cost pennies; XR can be 3–5 × more.
- Rapid titration needs. Clinicians can ramp IR from 500 mg to 2000 mg in small steps, adjusting every few days. XR jumps in 500–750 mg blocks.
- Renal monitoring. If kidney function is borderline, splitting IR into smaller doses lets you stop or dial back without wasting high-priced XR tabs.
When is XR the smarter pick?
- Persistent GI distress on IR despite slow titration.
- Once-daily lifestyle—perfect for people who already take evening meds for blood pressure or sleep.
- Adherence challenges. Fewer daily doses equals fewer missed doses, a point not to underestimate.
Ultimately, many patients start on IR (cheap, flexible) and switch to XR if side-effects nag or schedules get messy. If insurance covers XR at the same tier — or with a modest copay differential — most clinicians prefer it for ease and comfort. Either way, the active ingredient is identical; what changes is the ride, not the destination.
Metformin for Weight Loss: Scientific Evidence and Real-World Cases
The increased interest in Metformin as a slimming aid stems from a simple observation: many people who take the medication lose small amounts of weight consistently, even when weight loss is not their primary goal. Metformin, unlike stimulants or GLP-1 agonists, nudges biology rather than controlling it, resulting in slower but longer-lasting weight reduction.
Large studies back up this view. In the Diabetes Prevention Program's 15-year follow-up, participants taking 1 700 mg/day of Metformin weighed on average 4% less than baseline—twice the loss of the lifestyle-only arm when age and adherence were taken into account. Meta-analyses of PCOS and non-diabetic obesity suggest an average weight loss of 2-5 kg over 6-12 months, with better results in those who are already severely insulin resistant.
Dosing is crucial. The majority of weight-focused studies titrated to 1 500-2 000 mg per day (split BID or QHSXR). Lower doses improve glucose levels but seldom shift the scale. Experts, on the other hand, urge that metformin be used in conjunction with calorie management and frequent exercise because the medication improves rather than substitutes these behaviors.
Real-world data supports the experiments. A primary-care registry of 10,000 people in the United Kingdom discovered a 4.3 kg mean weight loss at one year that stayed (3.1 kg) at year three; patients who walked at least 150 minutes per week kept almost all of their weight off. Importantly, gastrointestinal discomfort predicted greater weight loss — possibly as a proxy for more appetite suppression — but the majority of symptoms resolved within six weeks.
Personal stories provide texture. Alicia, 42, BMI 32, prediabetic, cut sugary snacks and started taking 1 500 mg XR in the evening; she dropped 9 kg in eight months and reported "no wild cravings by 3 p.m." Sam, a 55-year-old night-shift nurse, lost 6 kg in four months by combining 850 mg BID with high-protein meals and managing his blood pressure without the need of extra drugs.
Bottom line: Metformin will not generate the dramatic curves seen with newer injectable drugs, but for patients who tolerate it, the combination of modest appetite control, lower insulin levels, and low cost makes it a great first step toward weight management.
How Metformin Affects Appetite and Eating Behavior
Metformin lowers appetite by lowering insulin peaks. When insulin levels remain moderate rather than rising, downstream hunger hormones like neuropeptide Y are inhibited, reducing the "I need a snack now" signal.
GLP-1, produced in the stomach, is a secondary lever. According to studies, metformin increases endogenous GLP-1 by 20-30%, prolonging sensations of fullness after meals — milder than injectable agonists, but enough that many users reduce their portion sizes automatically.
Early-phase gastrointestinal side effects (moderate nausea, metallic taste) discourage thoughtless snacking. Surprisingly, the impact lasts even after the discomfort has passed, indicating a learnt behavior: users become acclimated to smaller meals and never fully return to pre-metformin portion proportions.
- “I used to raid the fridge every night. Two weeks into 500 mg BID metformin, the urge just wasn’t there.” — Jane, 34
- “No jittery appetite suppression—more like my stomach finally sends the ‘full’ signal on time.” — Mark, 52
- “Lost 3 kg without realizing because I stopped finishing the kids’ leftovers.” — Priya, 40
Finally, Metformin may alter the gut microbiota to favor species linked with thinner phenotypes (such as Akkermansia muciniphila). Though causative routes are still being researched, preliminary research indicates that bacterial diversity and self-reported satiety change concurrently.
Clinicians advocate taking the medicine with protein-rich meals and at consistent meal times for best results. That regimen synchronizes metformin's pharmacokinetics with natural satiety waves, converting a little biochemical benefit into a substantial daily calorie decrease.
Metformin Side Effects: Common Issues and How to Minimize Them
Metformin’s safety record is strong, yet almost everyone feels some “settling-in” turbulence. The drug is processed in the gut, filtered by the kidneys, and circulated in nearly every tissue, so its side-effect map spreads across several body systems.
1. Gastrointestinal (the classic hiccup)
Loose stools, mild nausea, gassy bloating, or a metallic taste typically appear in the first two weeks. Slow titration, taking tablets mid-meal, and switching to extended-release (XR) formulations curb these problems in >70 % of users.
2. Vitamin B12 Drain
Long-term therapy can trim B12 stores by 10–20 %. Most people stay above deficiency thresholds, but vegetarians or older adults should add a daily 500 µg oral supplement or check serum levels every 12–18 months.
3. Mild Appetite Dip & Fatigue
Lower insulin peaks blunt hunger but can also trigger early-afternoon sluggishness during the first month. Balancing each dose with at least 15 g of protein (e.g., Greek yogurt or a boiled egg) smooths energy curves.
4. Rare but Serious: Lactic Acidosis
This event occurs roughly 3 in 100 000 patient-years—mostly in people with advanced kidney or liver disease, severe dehydration, or acute heart failure. Checking eGFR every 6–12 months and pausing metformin 48 h before iodinated contrast studies keeps risk vanishingly small.
5. Skin & Taste Oddities
About 1 % report rash, itching, or persistent metallic tongue. These generally fade after dose reduction; otherwise, a switch to another first-line agent is prudent.
Safe-Start Rules for Metformin
- Start at 500 mg with the largest meal for one week
- Step up by 500 mg only if GI symptoms are mild
- Always take tablets with food and a full glass of water
- Consider XR if discomfort lasts > 14 days
- Check B12 yearly if on > 1 000 mg/day or following a vegan diet
- Pause metformin during severe dehydration, surgery, or IV contrast scans
If side-effects persist despite these adjustments, discuss dosage spacing (e.g., 500 mg breakfast, 1 000 mg dinner) or an alternative such as GLP-1 agonists—especially when weight loss is a priority.
Is Metformin Compatible with Other Medications? Interactions and Risks
Metformin plays well with most drugs because it isn’t metabolized by the liver’s CYP enzymes. Still, certain combinations can amplify side-effects or mask trouble. Think in families rather than single agents.
Other Glucose-Lowering Drugs – Pairing Metformin with insulin or sulfonylureas (glipizide, glyburide) deepens glucose control but raises hypoglycemia risk. Solution: start combo therapy at 25–50 % of the usual insulin/sulfonylurea dose and adjust by finger-stick readings.
Diuretics and ACE/ARB Antihypertensives – High-dose loop diuretics (Furosemide) increase dehydration and thus lactic-acidosis danger. ACE inhibitors (Lisinopril) mildly enhance insulin sensitivity, so watch for additive glucose drops during the first fortnight.
Contrast Media & Iodine Loads – Iodinated CT dyes can transiently dent kidney filtration. Current guidelines call for stopping Metformin the day of contrast and checking eGFR 48 h later; restart only if renal function returns to baseline.
Acid Suppressants & Cimetidine-Like Drugs – Cimetidine, and to a lesser extent ranitidine or famotidine, compete with metformin for renal tubular transport, nudging plasma levels 50 % higher. Reduce metformin or switch to a proton-pump inhibitor if chronic H2 blockers are necessary.
Corticosteroids & Atypical Antipsychotics – These raise blood sugar. Metformin can blunt but not fully counteract the spike; clinicians often boost metformin to the 2 000 mg/day range or add a second agent during steroid bursts.
Topiramate & Carbonic-Anhydrase Inhibitors – Combined use slightly raises lactic-acidosis risk via acid–base shifts. Monitor serum bicarbonate if both drugs are essential.
Alcohol – Moderate intake (≤ 2 standard drinks/day) rarely interacts. Binge drinking, however, hampers liver gluconeogenesis and dehydrates—two hits that can trigger lactic acidosis. Best practice: skip Metformin on any day involving heavy alcohol or vomiting, hydrate, and restart 24 h after the last drink.
In short, Metformin’s interaction slate is manageable: keep kidneys hydrated, double-check renal labs during new medication starts, and pause therapy around contrast dye or drunken weekends. The payoff is seamless integration with most chronic-care regimens—all while keeping glucose and insulin on a shorter leash.
Metformin Against Insulin Resistance: Mechanism, Indications, and Effectiveness
Insulin resistance (IR) starts quietly: muscle, liver, and fat cells stop "listening" to normal insulin signals, prompting the pancreas to release more of the hormone. Blood sugar levels can remain normal for months or years, but chronically increased insulin promotes weight gain, tiredness, and, eventually, pre-diabetes. Metformin tackles this dynamic on three levels: cellular energy sensing, hepatic glucose management, and gut hormone modulation — long before full-blown diabetes occurs.
At the molecular level, Metformin activates AMP-activated protein kinase (AMPK), a metabolic switch that encourages cells to burn available energy rather than generating new fat. When AMPK is active, glucose transporters (GLUT-4) move to the cell surface, allowing sugar to enter without requiring extra insulin. Metformin inhibits hepatic gluconeogenesis, leading the liver to produce less glucose into the bloodstream during fasting hours, resulting in decreased glucose and insulin demand.
If fasting insulin levels surpass 10 µIU/mL or HOMA-IR values exceed 2.5, doctors may prescribe Metformin, especially if lifestyle adjustments have not been beneficial. Women with PCOS, who are gaining weight mostly around the waist, and those on steroids or atypical antipsychotics are suitable candidates. Because the medicine seldom causes hypoglycemia, it is safe to start even if fasting glucose is "normal" but increasing.
- First-line choice when HOMA-IR > 2.5 and BMI ≥ 27 kg/m²
- Add-on therapy for PCOS with anovulation or hirsutism
- Preventive use after gestational diabetes to curb future IR
- Adjunct option during chronic corticosteroid treatment
The efficacy is high. A network meta-analysis of 30 trials found that Metformin lowered fasting insulin by 25-30% and improved HOMA-IR by 1-1.5 points in six months, which is comparable to rigorous exercise regimens. When combined with calorie counting and 150 minutes of weekly walking, the average weight loss was 4-6 kg, much outweighing lifestyle changes alone. Importantly, benefits peak around 2,000 mg/day; higher doses seldom add value and instead produce gastrointestinal irritation.
The side-effect profiles in IR patients are comparable to those in diabetic care, with the majority of symptoms being transient. Regular B12 testing and renal labs guarantee that long-term treatment runs properly. For many, the benefits are tangible: more steady energy, less post-meal crashes, and a slow but considerable drop in waist circumference during the first year.
Metformin and Future Outlook for Insulin Resistance
Starting Metformin is usually the turning moment, not the end line. Long-term registries demonstrate that patients who take the medicine and make moderate lifestyle changes reduce their chance of developing type 2 diabetes by 31% over a decade, even if they do not lose significant weight. Cardiovascular outcomes also improve; observational data show that long-term Metformin use is associated with a 15-20% reduced risk of heart attack than matched nonusers.
A new study suggests that there may be further advantages. Metformin may slow the advancement of NAFLD and maybe decrease cancer risks by reducing chronic inflammation and gut microbiota diversity, while conclusive research is still being conducted. Scientists are now looking on low-dose "maintenance" regimens (250-500 mg XR weekly) that might help preserve insulin sensitivity and prevent GI difficulties if major weight goals are accomplished.
Patient experiences underscore these numbers:
“Six months in, my fasting insulin dropped from 22 to 11 µIU/mL. I haven’t reached my goal weight yet, but my energy doesn’t crash at 3 p.m. anymore.” — Lena, 38
“I paired 1 000 mg XR with strength training. Lost only 5 kg, yet my A1c slid from 5.8 % to 5.2 % and my HDL went up.” — Carlos, 45
Looking ahead, combination therapies are gaining traction. Small trials combining Metformin with berberine, inositol, or low-dose GLP-1 agonists reveal synergistic decreases in fasting insulin levels without extra side effects. Personalized therapy is also on the horizon, with pharmacogenomic testing possibly predicting who responds better to metformin than other choices like pioglitazone or SGLT2 inhibitors.
Patients who are already in therapy have a mostly self-centered perspective. Consistency — taking pills with meals, documenting weekly fasting glucose, and rechecking labs every six months — helps keep momentum. Most people discover that as their cravings subside and their energy levels normalize, sticking to their eating and exercise goals becomes simpler, resulting in a positive feedback loop that enhances insulin sensitivity.
In short, Metformin is not a cure-all, but it is a solid basis. When combined with modest lifestyle adjustments and regular monitoring, it offers a viable path for overcoming early insulin resistance and delaying — or maybe avoiding — the diabetes on-ramp for years.
Can You Take Metformin Without Diabetes? An Endocrinologist’s Answer
Endocrinologists are increasingly recommending Metformin to patients who do not have a formal diabetes diagnosis but fall into the metabolic "gray zone" - prediabetes, insulin resistance, polycystic ovarian syndrome (PCOS), or persistent central weight gain. The rationale is threefold: it lowers fasting insulin, smoothes post-meal glucose peaks, and, unlike many newer medications, has a decades-long safety record at a fair price.
However, experts make it clear that Metformin is not a health supplement. They recommend baseline testing (fasting glucose, insulin, eGFR, and B12) as well as a particular treatment goal, such as reducing HOMA-IR, encouraging ovulatory cycles in PCOS, or delaying the progression to type 2 diabetes, according to the Diabetes Prevention Program. Random "bio-hacking" without labs or follow-up raises the possibility of missing B12 deficiency or silent renal impairment.
The hazards remain small yet genuine. GI discomfort affects around one-in-five starters. After 12 months, a monthly B12 check is indicated. Those with eGFR < 45 mL/min/1.73 m² should avoid or reduce the medication. For women with PCOS, benefits frequently include a modest weight loss (2-5 kg over six months), lower triglycerides, and tighter cycle consistency. Most endocrinologists believe that a motivated patient undergoing medical treatment has a favorable risk-benefit ratio. Self-prescription of "energy" or "focus" is more difficult to justify.
Metformin and Physical Exercise: Can It Support Your Workouts?
Metformin's effect on training is minimal. By lowering baseline insulin levels, the medication can make fat storage more accessible during steady-state activity, resulting in "lighter legs" during long runs. Small crossover trials show that after four weeks on 1,500 mg XR, trained cyclists metabolize more fat and less carbohydrate, with no effect on VO2max.
However, strong athletes should use caution. A well-cited 2019 study in Aging Cell found that older persons who took Metformin and progressive resistance training had 20% less lean muscle than placebo lifters, most likely due to AMPK activation inhibiting mTOR signaling. This does not cancel out the medicine, but lifters seeking maximal hypertrophy may opt to schedule the dosage after a workout or take XR before bedtime to minimize acute interaction.
Athlete snapshot
- “Switched from 500 mg BID to 1 000 mg XR nightly. Long runs feel steadier, fewer gel cravings.”— Cara, marathoner, 33
- “Gained strength but plateaued on muscle size; dropping morning dose fixed it.” — Jamal, CrossFit coach, 40
Practical tips: keep hydration high (Metformin is mildly diuretic); ingest 15–25 g protein with the dose to reduce nausea; and schedule heavy lifts at least six hours after an IR tablet if maximal anabolic signaling is the goal.
Metformin and Autonomic Symptoms: Can It Help with Chronic Fatigue?
Chronic fatigue is typically connected with abnormal glucose swings and low-grade inflammation. Metformin can help to normalize autonomic symptoms such midday crashes, brain fog, and moderate orthostatic dizziness by smoothing out variations. Pilot investigations in post-viral fatigue cohorts show small but significant increases in the Fatigue Impact Scale after 12 weeks at 1,000 mg/day.
However, physicians warn against taking Metformin as a "pick-me-up" medication. Sleep hygiene, proper macronutrient intake, and graded exercise remain major concerns. Metformin simply decreases metabolic noise, making lifestyle modifications more likely to last.
- Helpful when fatigue tracks high fasting insulin (> 10 µIU/mL)
- Less effective if fatigue stems from iron/B12 deficiency or thyroid issues
- Start low (500 mg dinner) and reassess energy after four weeks
Bottom line: the medication may smooth peaks and valleys, but revamping sleep, stress, and nutrient status determines long-term stamina.
The Anti-Aging Effect of Metformin: Myth or Biomedical Breakthrough?
Metformin's popularity as a longevity medicine soared after epidemiological studies demonstrated that diabetics who took metformin lived as long — if not longer — than non-diabetic controls. Animal studies support the hypothesis: mice fed metformin have improved mitochondrial efficiency, decreased oxidative stress, and a longer median lifespan.
The TAME research (Targeting Aging with Metformin) is the definitive human test, with 3,000 non-diabetic adults aged 65-79 being followed for major age-related events (heart attack, stroke, cancer, dementia). Results are expected later this decade, and preliminary pharmacokinetic data support the safety of 1 500 mg XR daily in older people.
Skeptics argue that Metformin's benefits may be related to improved metabolic profiles rather than anti-aging properties. Nevertheless, early adopters are vocal:
“My CAC score stayed flat for four years, and my A1c dropped from 5.7 % to 5.3 %.” — Greg, 66
“Skin looks clearer; joint aches down after six months on 850 mg XR nightly.” — Mira, 59
Potential drawbacks include lower gains from high-intensity resistance training and perhaps vitamin B12 insufficiency. Until TAME is completed, most geroscience practitioners reserve metformin for patients with metabolic risk factors, advising healthy normoglycemic people to focus protein-rich meals, HIIT, and enough sleep.
Conclusion: promising, but unproven. Metformin may slow the aging process, but it is unlikely to replace crucial lifestyle variables.